Brain fog reflects that your brain may not be healthy enough to function at its best. To address it, you need to take into account all of the reasons brain fog exists. Also, each case of brain fog is different, which is why we ensure that our stacks are personalized.
This article, part 1, will cover the different contributors to brain fog. In the next article, part 2, we will cover how Nootopia’s personalized nootropics can eliminate brain fog and catapult you into your apex performance.
Contributors To Brain Fog

To put an end to brain fog, you first have to know what causes it. Your brain needs appropriate nutrients, optimal brain metabolism, and healthy neurotransmitter levels.
In addition, to function at a high level consistently, you need to keep inflammation and oxidative stress in check. Keep in mind that brain fog can also be a symptom of more severe conditions, so you want to consult your medical provider to rule these out first.
Many people still feel brain fog despite being deemed healthy. While brain fog is very common, we believe that it’s far from healthy. The following are the primary contributors to brain fog and are areas that Nootopia addresses.
Low Acetylcholine
Acetylcholine (ACh) is a foundational neurotransmitter for memory, focus, and more. Outside the brain and central nervous system, ACh is the primary stimulating/excitatory neurotransmitter. However, in the brain, ACh functions more as a neuromodulator. The primary functions of ACh in the brain are:
- Alters how sensitive or excitable neurons are to other signals
- Modulates the release of other neurotransmitters
- Coordinates the collective firing of groups of neurons
Neurons that release ACh are found throughout the entire central nervous system, affecting all areas of the brain. Healthy ACh function is particularly important for learning, memory, and attention, making it a primary target to get rid of brain fog.
Low acetylcholine may also affect the vagus nerve, contributing to whole-body inflammation.
Neuroinflammation
Neuroinflammation is inflammation present anywhere in the central nervous system (brain and spinal cord). As with inflammation in the rest of the body, it’s normal and natural to have some low and temporary inflammation in your brain.
Chronic neuroinflammation however, is particularly detrimental to brain health and function. Brain fog is one symptom of neuroinflammation, due largely to the downstream effects of elevated immune system messengers (cytokines).
Other common manifestations of neuroinflammation include:
- Damage to cells in and around the area of
inflammation. Whatever function these neurons
carry out is then compromised.
- Anxiety
- Depression
- Cognitive impairment
- Decreased neural plasticity, or the ability of your nervous system to adapt and change in response to internal or external factors
Neuroinflammation can be caused by a single or a constellation of factors including:
- Chronic stress
- Emotional trauma
- Physical trauma, such as head injury
- Infection, both inside and outside the brain
- Exposure to certain environmental toxins, like heavy metals
- Mold exposure/mycotoxins
- Normal aging
- Leaky gut
- Leaky blood brain barrier
Leaky Blood Brain Barrier
The blood-brain barrier (BBB) is the barrier between your bloodstream and your brain. It is a primary control point for determining what enters the brain and what is excluded. The BBB is very selective about what gets across. A healthy BBB has receptors to allow certain molecules to cross. Very small substances and fat soluble molecules typically will make it across the barrier as well.
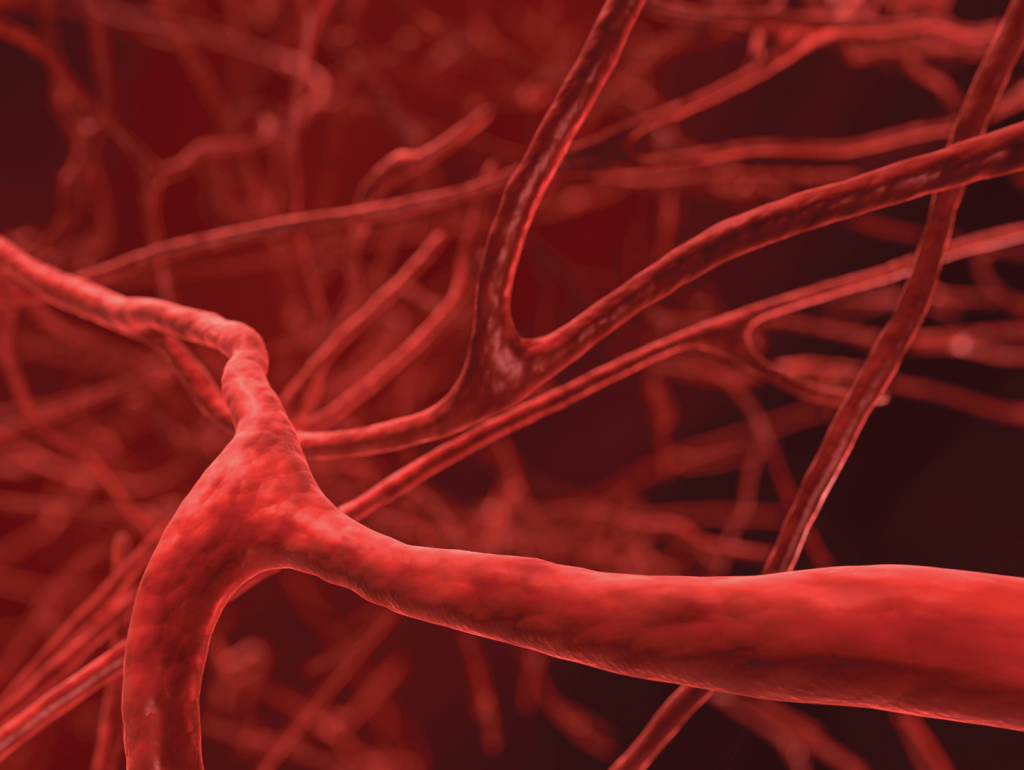
If the BBB becomes leaky, substances that would normally be excluded from entering the brain can cross. Other molecules that would have crossed in a controlled manner are now able to flood in as well. It is a lot like leaky gut, only of the brain.
Leaky BBB results in a host of neurologic dysfunctions and neuroinflammation. Inflammation increases BBB permeability, which increases neuroinflammation, which further increases leaky BBB. This creates a cycle of dysfunction.
Symptoms and health conditions associated with leaky BBB include:
- Brain fog
- Depression
- Neurodegenerative diseases (Alzheimer’s, Multiple sclerosis, etc.)
- Autism
- Seizures
- Schizophrenia
While researchers have uncovered many BBB breachers, they’re still trying to understand the exact processes. All of these factors are associated with leaky BBB and may contribute to its development.
- Systemic (whole-body) inflammation
- Heavy metal toxicity
- Leaky gut
- Sleep-wake cycle disruption
- Stress
- Bacterial infection
- High homocysteine levels
- Blood sugar imbalance/hyperglycemia
- Mold toxins (mycotoxins)
Low Brain Metabolism Or Poor Mitochondrial Function
When your brain cells don’t produce enough energy, it becomes difficult to think clearly and focus. Low brain metabolism causes poor mental performance and brain fog.
Some reasons for low brain metabolism include:
- Decreased cerebral blood flow
- Insulin resistance
- Mitochondrial dysfunction
- Low thyroid function
- Hypoxia or low oxygen delivery to the brain, such as in sleep apnea or anemia
The metabolic pathways of brain cells also need adequate cofactors in order to produce enough energy. Some cofactors required for cellular energy production are B vitamins, CoQ10, and Alpha-lipoic acid (ALA).
High Oxidative Stress
Along with inflammation, oxidative stress is most likely the cause of brain fog. Brain cells are particularly susceptible to oxidative stress because of their high oxygen use. Oxidative stress may be caused by other factors, such as leaky BBB and inflammation. However, most of the contributors to brain fog end up resulting in increased oxidative burden on the brain.
Oxidative stress damages mitochondria and triggers inflammation pathways. The lipid membranes of neurons can be damaged by oxidative stress as well. This causes cell dysfunction and potentially cell death.
Oxidative stress can cause the mitochondria to slow down to protect your cells from more oxidative stress. It’s natural to have high oxidative stress at night in order to sleep. However, other persistent lifestyle-related oxidative stress can cause daytime fatigue and the “cloudy head” sensation common in brain fog.
Stress
Your brain needs some stress as stimuli to stay alive and grow. However, the inability to enter a parasympathetic state or constant stress reactivity can cause brain fog.
Chronic, unmanaged stress leads to poor brain function all around. These may include emotional, social, and cognitive functioning. Stress decreases the capability of neurons to send signals appropriately. What’s worse is that stress causes a loss of neurons and can actually cause the brain to shrink.

Chronic stress and trauma can cause chronic activation of the sympathetic nervous system (fight or flight) and the hypothalamic-pituitary-adrenal (HPA) axis. This decreases cerebral blood flow to crucial areas of cognitive function such as the hippocampus. It can even cause the wrong kind of brain rewiring towards more stress reactivity.
Men are particularly vulnerable to memory impairment from chronic stress due to changes in the hypothalamus.
Nutrient Deficiencies
Besides the vitamins and minerals that support mitochondrial function, there are other vital nutrients necessary for healthy brain function and eliminating brain fog. These are some of the most important nutrients for brain health.
Omega-3 Fatty Acids
The brain is made up of nearly 60% lipids (fats). Omega-3 essential fatty acids (EFA) provide healthy structure to neurons and keep cell membranes healthy and fluid. EFA’s also act as cell messengers and are involved in the production of neurotransmitters.
Omega-3’s may improve brain fog, including attention and memory.
Healthy levels of omega-3 fatty acids are neuroprotective.
Magnesium
Magnesium is a cofactor in metabolic and neurotransmitter functions in the brain. Low or suboptimal magnesium levels are associated with poor cognitive performance. People with higher magnesium levels have better attention and memory performance, and less likelihood of developing cognitive impairment.
Low magnesium levels may also predispose anxiety, depression, and decreased stress resilience. These each negatively impact cognition and contribute to brain fog.
Vitamin B12
Vitamin B12 plays an irreplaceable role in the nervous system. As a vitamin cofactor, B12 is required for the production of the myelin sheath around nerves. This makes nerve conduction efficient and effective.
Low B12 manifests as a number of potentially irreversible nervous system symptoms, including:
- Cognitive impairment
- Numbness and tingling in extremities
- Headaches
- Tinnitus (ringing in the ears)
Vitamin D
Vitamin D promotes cognitive function, including learning and memory.
Low vitamin D levels can affect mood, and mood changes are associated with brain fog. Mood stabilization may be a primary means that vitamin D supports cognitive performance.
Poor Sleep Or Lack Of Sleep
Everyone has experienced the way the brain functions on little or poor quality sleep. Sleep deprivation increases the risk for chronic disease. It causes brain dysfunction that results in impaired decision-making and increased risk for motor vehicle accidents.
Inadequate sleep impairs the signaling between neurons and leads to momentary “cognitive lapses.” These lapses impact memory and visual perception.

Too Much Of The Wrong Stimulants
Stimulants, such as caffeine, can have various effects from person to person. Your genetics have a lot to do with this. Some people can process and metabolize stimulants relatively efficiently, while others are poor metabolizers.
If you have genetics that keep you from processing and eliminating stimulants well, they tend to cause jitters that inhibit cognitive function. This is why some people are sensitive to even small amounts of coffee, for example.
For these folks, too much stimulants may actually cause brain fog. Caffeine and other stimulants are also vasoconstricting and may decrease cerebral blood flow.
Conclusion
Brain fog is not a nootropic deficiency. To successfully eliminate brain fog and enable your brain to function in all cylinders, most people need a comprehensive approach that goes beyond conventional nootropics. Also, every case of brain fog is different, so a one-size fits all approach can work great for one person and worsen brain fog for another.
Try our quiz here to find out what stack works best for you.
In our next article, part 2, we’ll cover how Nootopia’s personalized nootropic stacks uniquely help with brain fog.
References:
- Picciotto MR, Higley MJ, Mineur YS. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron. 2012;76(1):116-129. doi:10.1016/j.neuron.2012.08.036
- Breit S, Kupferberg A, Rogler G, Hasler G. Vagus nerve as modulator of the brain–gut axis in psychiatric and inflammatory disorders. Front Psychiatry. 2018;9. doi:10.3389/fpsyt.2018.00044
- DiSabato DJ, Quan N, Godbout JP. Neuroinflammation: the devil is in the details. J Neurochem. 2016;139(Suppl 2):136-153. doi:10.1111/jnc.13607
- Theoharides TC, Stewart JM, Hatziagelaki E, Kolaitis G. Brain “fog,” inflammation and obesity: key aspects of neuropsychiatric disorders improved by luteolin. Front Neurosci. 2015;9:225. doi:10.3389/fnins.2015.00225
- Li L, Mao S, Wang J, Ding X, Zen JY. Viral infection and neurological disorders—potential role of extracellular nucleotides in neuroinflammation. ExRNA. 2019;1(1):1-5. doi:10.1186/s41544-019-0031-z
- Bondy SC. Metal toxicity and neuroinflammation. Curr Opin Toxicol. 2021;26:8-13. doi:10.1016/j.cotox.2021.03.008
- Baizabal-Carvallo JF, Alonso-Juarez M. The link between gut dysbiosis and neuroinflammation in parkinsońs disease. Neuroscience. 2020;432:160-173. doi:10.1016/j.neuroscience.2020.02.030
- Najjar S, Pearlman DM, Devinsky O, Najjar A, Zagzag D. Neurovascular unit dysfunction with blood-brain barrier hyperpermeability contributes to major depressive disorder: a review of clinical and experimental evidence. J Neuroinflammation. 2013;10(1):142. doi:10.1186/1742-2094-10-142
- Gudmundsson P, Skoog I, Waern M, et al. The relationship between cerebrospinal fluid biomarkers and depression in elderly women. Am J Geriatr Psychiatry. 2007;15(10):832-838. doi:10.1097/JGP.0b013e3180547091
- Zenaro E, Piacentino G, Constantin G. The blood-brain barrier in Alzheimer’s disease. Neurobiol Dis. 2017;107:41-56. doi:10.1016/j.nbd.2016.07.007
- Ortiz GG, Pacheco-Moisés FP, Macías-Islas MÁ, et al. Role of the blood-brain barrier in multiple sclerosis. Arch Med Res. 2014;45(8):687-697. doi:10.1016/j.arcmed.2014.11.013
- Fiorentino M, Sapone A, Senger S, et al. Blood–brain barrier and intestinal epithelial barrier alterations in autism spectrum disorders. Mol Autism. 2016;7(1). doi:10.1186/s13229-016-0110-z
- Theoharides TC, Zhang B. Neuro-inflammation, blood-brain barrier, seizures and autism. J Neuroinflammation. 2011;8(1):168. doi:10.1186/1742-2094-8-168
- van Vliet EA, Aronica E, Gorter JA. Blood-brain barrier dysfunction, seizures and epilepsy. Semin Cell Dev Biol. 2015;38:26-34. doi:10.1016/j.semcdb.2014.10.003
- Najjar S, Pahlajani S, De Sanctis V, Stern JNH, Najjar A, Chong D. Neurovascular unit dysfunction and blood-brain barrier hyperpermeability contribute to schizophrenia neurobiology: A theoretical integration of clinical and experimental evidence. Front Psychiatry. 2017;8:83. doi:10.3389/fpsyt.2017.00083
- Müller N, Ackenheil M. Immunoglobulin and albumin content of cerebrospinal fluid in schizophrenic patients: relationship to negative symptomatology. Schizophr Res. 1995;14(3):223-228. doi:10.1016/0920-9964(94)00045-a
- Varatharaj A, Galea I. The blood-brain barrier in systemic inflammation. Brain Behav Immun. 2017;60:1-12. doi:10.1016/j.bbi.2016.03.010
- Banks WA. The blood-brain barrier: connecting the gut and the brain. Regul Pept. 2008;149(1-3):11-14. doi:10.1016/j.regpep.2007.08.027
- Kelly JR, Kennedy PJ, Cryan JF, Dinan TG, Clarke G, Hyland NP. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015;9:392. doi:10.3389/fncel.2015.00392
- He J, Hsuchou H, He Y, Kastin AJ, Wang Y, Pan W. Sleep restriction impairs blood-brain barrier function. J Neurosci. 2014;34(44):14697-14706. doi:10.1523/JNEUROSCI.2111-14.2014
- Esposito P, Gheorghe D, Kandere K, et al. Acute stress increases permeability of the blood-brain-barrier through activation of brain mast cells. Brain Res. 2001;888(1):117-127. doi:10.1016/s0006-8993(00)03026-2
- Leppert D, Leib SL, Grygar C, Miller KM, Schaad UB, Holländer GA. Matrix metalloproteinase (MMP)-8 and MMP-9 in cerebrospinal fluid during bacterial meningitis: association with blood-brain barrier damage and neurological sequelae. Clin Infect Dis. 2000;31(1):80-84. doi:10.1086/313922
- Beard RS Jr, Reynolds JJ, Bearden SE. Hyperhomocysteinemia increases permeability of the blood-brain barrier by NMDA receptor-dependent regulation of adherens and tight junctions. Blood. 2011;118(7):2007-2014. doi:10.1182/blood-2011-02-338269
- Prasad S, Sajja RK, Naik P, Cucullo L. Diabetes mellitus and blood-brain barrier dysfunction: An overview. J Pharmacovigil. 2014;2(2):125. doi:10.4172/2329-6887.1000125
- Hope J. A review of the mechanism of injury and treatment approaches for illness resulting from exposure to water-damaged buildings, mold, and mycotoxins. ScientificWorldJournal. 2013;2013:767482. doi:10.1155/2013/767482
- Talarowska M, Bobińska K, Zajączkowska M, Su KP, Maes M, Gałecki P. Impact of oxidative/nitrosative stress and inflammation on cognitive functions in patients with recurrent depressive disorders. Med Sci Monit. 2014;20:110-115. doi:10.12659/MSM.889853
- Bhat AH, Dar KB, Anees S, et al. Oxidative stress, mitochondrial dysfunction and neurodegenerative diseases; a mechanistic insight. Biomed Pharmacother. 2015;74:101-110. doi:10.1016/j.biopha.2015.07.025
- Everson CA, Laatsch CD, Hogg N. Antioxidant defense responses to sleep loss and sleep recovery. Am J Physiol Regul Integr Comp Physiol. 2005;288(2):R374-83. doi:10.1152/ajpregu.00565.2004
- Ecole Polytechnique Fédérale de Lausanne. How stress tears us apart: Enzyme attacks synaptic molecule, leading to cognitive impairment. Science Daily. Published online September 18, 2014. Accessed September 28, 2022. https://www.sciencedaily.com/releases/2014/09/140918091418.htm
- Kang HJ, Voleti B, Hajszan T, et al. Decreased expression of synapse-related genes and loss of synapses in major depressive disorder. Nat Med. 2012;18(9):1413-1417. doi:10.1038/nm.2886
- Burrage E, Marshall KL, Santanam N, Chantler PD. Cerebrovascular dysfunction with stress and depression. Brain Circ. 2018;4(2):43-53. doi:10.4103/bc.bc_6_18
- Chang CY, Ke DS, Chen JY. Essential fatty acids and human brain. Acta Neurol Taiwan. 2009;18(4):231-241.
- Bauer I, Hughes M, Rowsell R, et al. Omega-3 supplementation improves cognition and modifies brain activation in young adults: Effects of omega-3 fatty acids on fMRI measures. Hum Psychopharmacol. 2014;29(2):133-144. doi:10.1002/hup.2379
- Stonehouse W, Conlon CA, Podd J, et al. DHA supplementation improved both memory and reaction time in healthy young adults: a randomized controlled trial. Am J Clin Nutr. 2013;97(5):1134-1143. doi:10.3945/ajcn.112.053371
- Al-Ghazali K, Eltayeb S, Musleh A, Al-Abdi T, Ganji V, Shi Z. Serum magnesium and cognitive function among Qatari adults. Front Aging Neurosci. 2020;12:101. doi:10.3389/fnagi.2020.00101
- Lo K, Liu Q, Madsen T, et al. Relations of magnesium intake to cognitive impairment and dementia among participants in the Women’s Health Initiative Memory Study: a prospective cohort study. BMJ Open. 2019;9(11):e030052. doi:10.1136/bmjopen-2019-030052
- Jaeger J. Digit Symbol Substitution Test: The case for sensitivity over specificity in neuropsychological testing: The case for sensitivity over specificity in neuropsychological testing. J Clin Psychopharmacol. 2018;38(5):513-519. doi:10.1097/JCP.0000000000000941
- Botturi A, Ciappolino V, Delvecchio G, Boscutti A, Viscardi B, Brambilla P. The role and the effect of magnesium in mental disorders: A systematic review. Nutrients. 2020;12(6):1661. doi:10.3390/nu12061661
- Katz MJ, Derby CA, Wang C, et al. Influence of perceived stress on incident amnestic mild cognitive impairment: Results from the Einstein Aging Study. Alzheimer Dis Assoc Disord. 2016;30(2):93-98. doi:10.1097/WAD.0000000000000125
- Pickering G, Mazur A, Trousselard M, et al. Magnesium status and stress: The vicious circle concept revisited. Nutrients. 2020;12(12):3672. doi:10.3390/nu12123672
- Jonsdottir IH, Nordlund A, Ellbin S, et al. Cognitive impairment in patients with stress-related exhaustion. Stress. 2013;16(2):181-190. doi:10.3109/10253890.2012.708950
- Castle M, Fiedler N, Pop LC, et al. Three doses of vitamin D and cognitive outcomes in older women: A double-blind randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2020;75(5):835-842. doi:10.1093/gerona/glz041
- Menon V, Kar SK, Suthar N, Nebhinani N. Vitamin D and depression: A critical appraisal of the evidence and future directions. Indian J Psychol Med. 2020;42(1):11-21. doi:10.4103/IJPSYM.IJPSYM_160_19
- Spedding S. Vitamin D and depression: a systematic review and meta-analysis comparing studies with and without biological flaws. Nutrients. 2014;6(4):1501-1518. doi:10.3390/nu6041501
- Vellekkatt F, Menon V. Efficacy of vitamin D supplementation in major depression: A meta-analysis of randomized controlled trials. J Postgrad Med. 2019;65(2):74-80. doi:10.4103/jpgm.JPGM_571_17
- Nir Y, Andrillon T, Marmelshtein A, et al. Selective neuronal lapses precede human cognitive lapses following sleep deprivation. Nat Med. 2017;23(12):1474-1480. doi:10.1038/nm.4433